Critical Care Crisis: Banner Health Pulls Plug on Northern Colorado ER Services
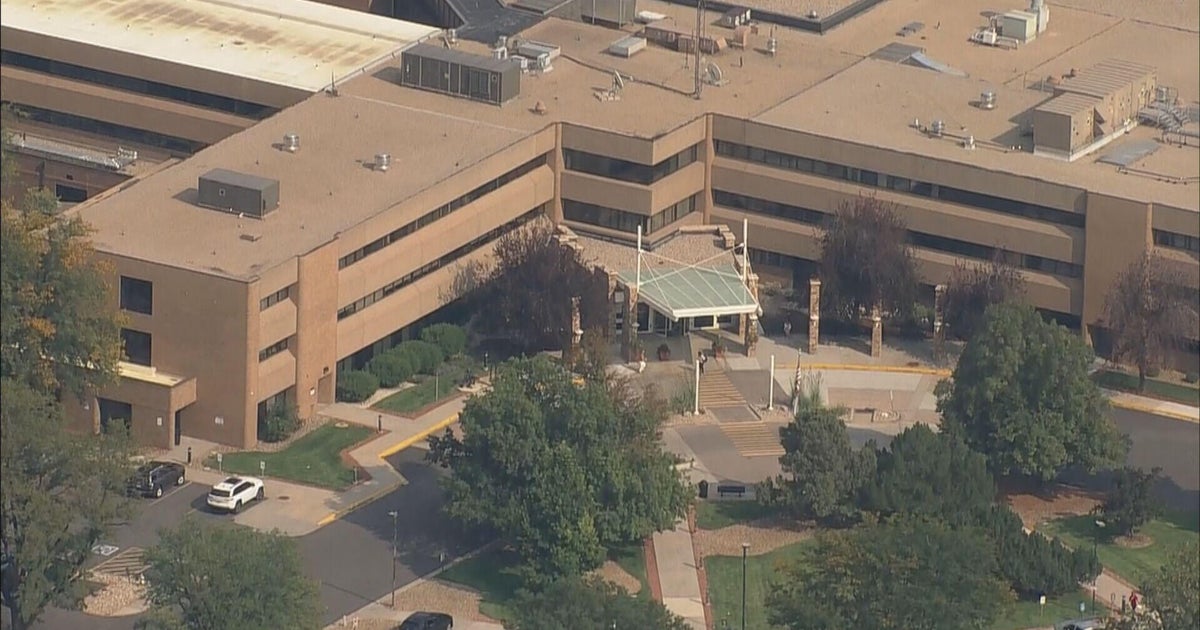
Patients and healthcare professionals at McKee Medical Center are bracing for significant changes as the hospital prepares to shutter its emergency room later this year. The Loveland facility's decision to close its emergency department has sparked concern among local residents who rely on the critical medical service.
Staff members have already been informed about the impending closure, which is expected to impact healthcare access for the surrounding community. While specific details about the reasons behind the closure remain limited, the announcement has raised questions about future emergency medical services in the area.
Local residents and healthcare workers are anxiously awaiting more information about how this closure will affect medical emergency response and where patients will be directed for urgent care needs. The hospital administration is anticipated to provide further details in the coming weeks about transition plans and alternative emergency medical resources.