Pharmacy Desert: Michigan's Vanishing Medical Lifelines and the Unexpected Saviors

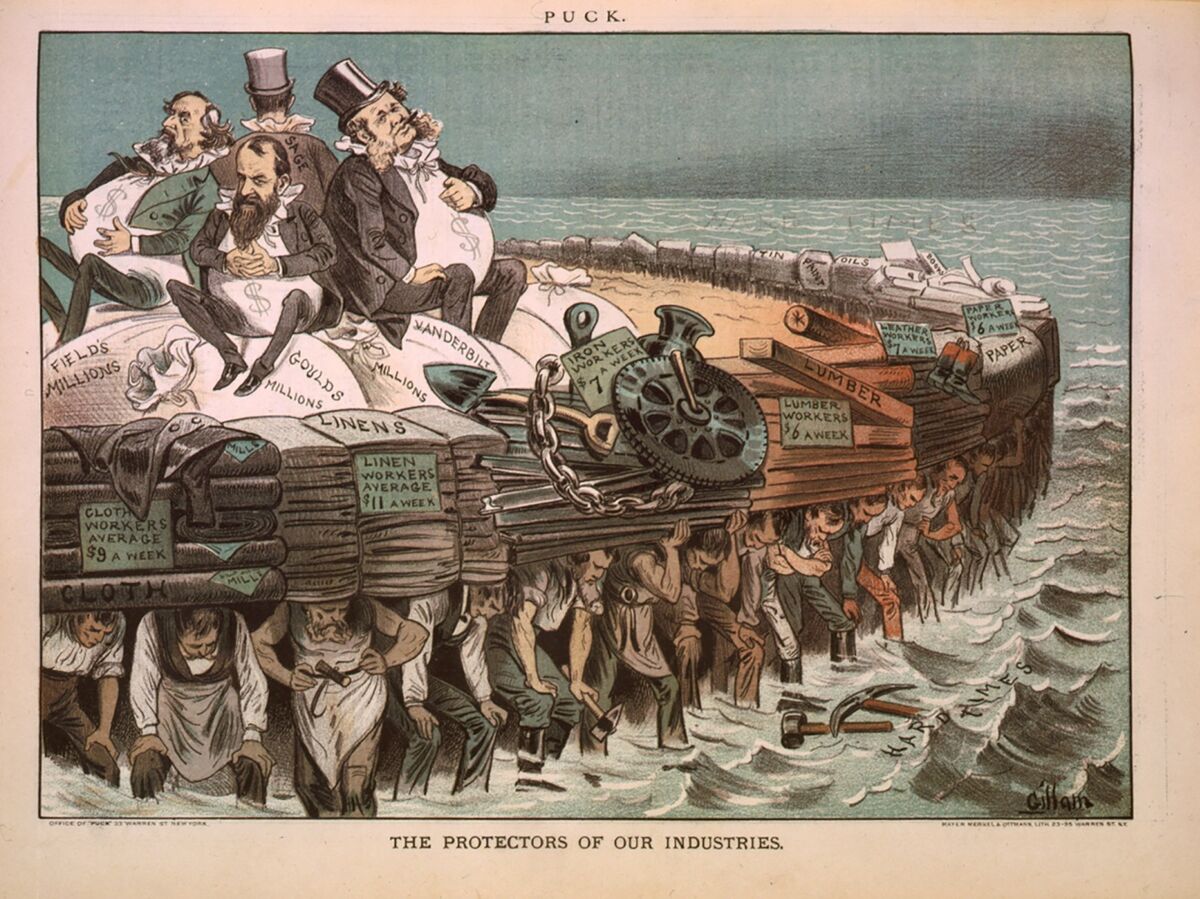
The landscape of pharmacy operations is undergoing significant challenges, with closures stemming from two primary factors: mounting corporate debt and controversial business strategies employed by pharmacy benefit managers (PBMs). These complex dynamics are reshaping the pharmaceutical retail sector, creating uncertainty for both businesses and consumers.
While some pharmacies are struggling under the weight of financial obligations, others find themselves navigating a challenging terrain dictated by the intricate practices of PBMs. These intermediaries, who negotiate drug prices and manage prescription benefits, have been increasingly scrutinized for their potential role in creating financial pressures for independent and chain pharmacies alike.
The intersection of corporate financial strain and PBM business models is creating a perfect storm that threatens the stability of pharmacy networks across the country. Pharmacies are being forced to adapt, consolidate, or in some cases, close their doors entirely, highlighting the urgent need for systemic reforms in the pharmaceutical distribution ecosystem.