Breaking: New England Launches Groundbreaking Public Health Guidelines
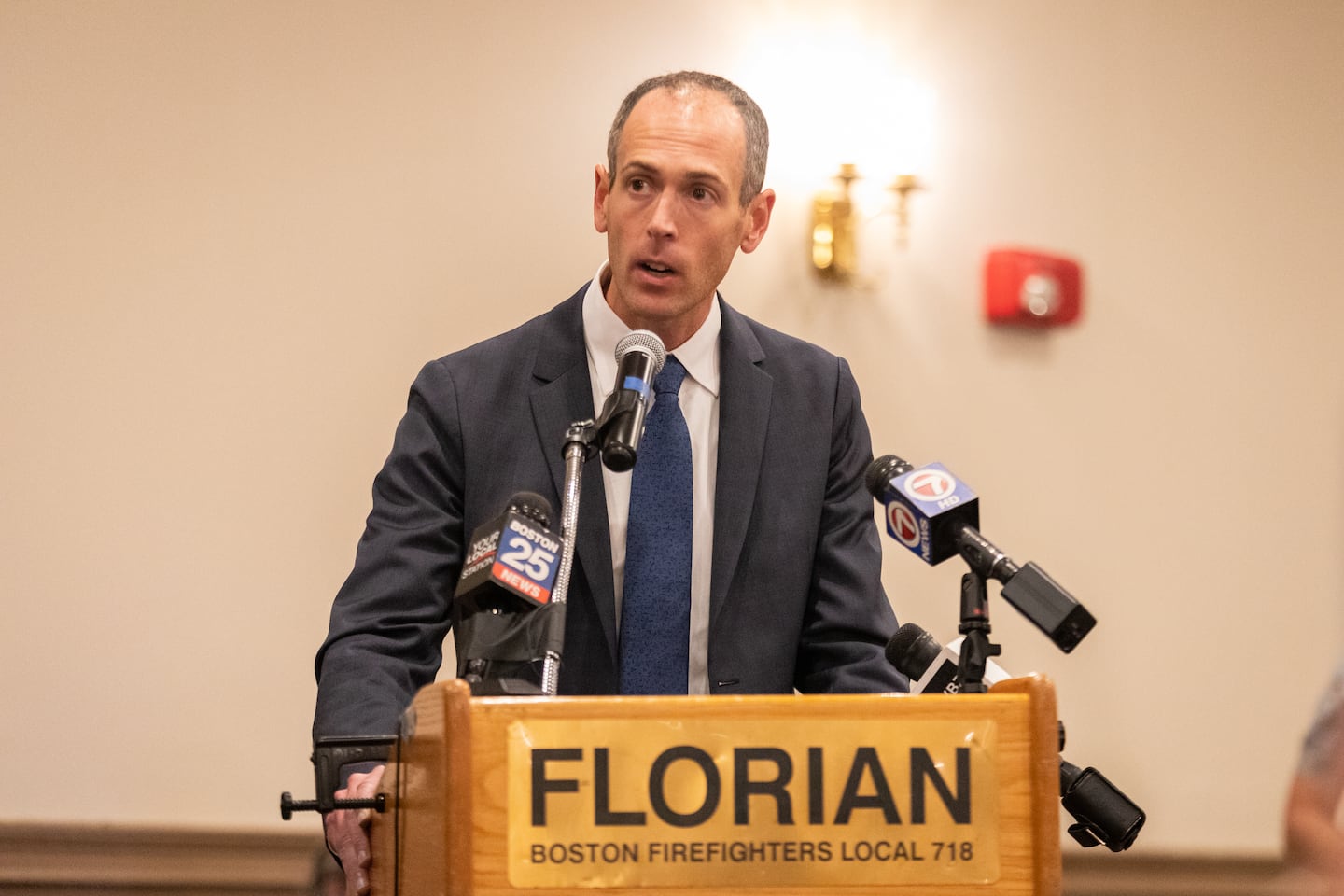
In a bold and decisive move, the state has officially severed ties with longstanding federal public health guidelines, signaling a dramatic shift in its approach to healthcare policy. This unprecedented decision represents a significant departure from established national protocols, highlighting the growing tension between local and federal health strategies.
By breaking away from traditional federal recommendations, the state is charting its own course in public health management. This strategic realignment suggests a desire for more localized, flexible healthcare solutions that can be tailored to the specific needs of the community.
The decision underscores a growing trend of states seeking greater autonomy in crafting health policies that they believe will more effectively address their unique demographic and medical challenges. It reflects a broader movement towards decentralized healthcare decision-making, where local authorities are increasingly empowered to take control of their public health strategies.
While the long-term implications of this break remain to be seen, it represents a bold statement of independence and a commitment to innovative, region-specific approaches to public health management.