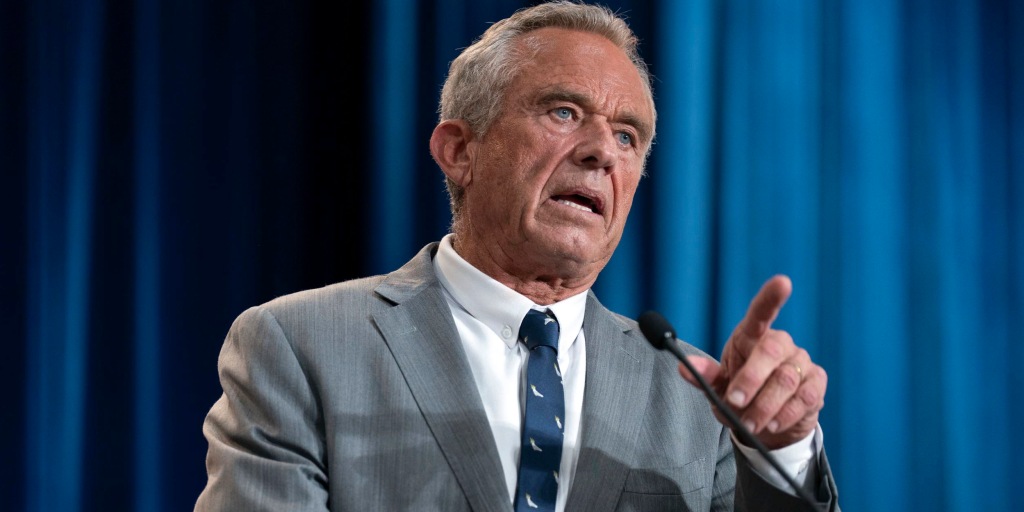
Urgent Probe: Democrats Grill Kennedy on 9/11 Health Program Delays

Struggling with persistent challenges, the program has been severely impacted by critical funding shortages and significant staffing reductions. These setbacks have created a frustrating bottleneck for survivors, who now face potentially months-long waiting periods just to secure a crucial initial appointment. The delays not only test the patience of those seeking support but also potentially compromise the timely assistance that can be vital in the healing process.