Breaking Barriers: How One Professor's Research Unveils Healthcare Challenges for Immigrant Communities
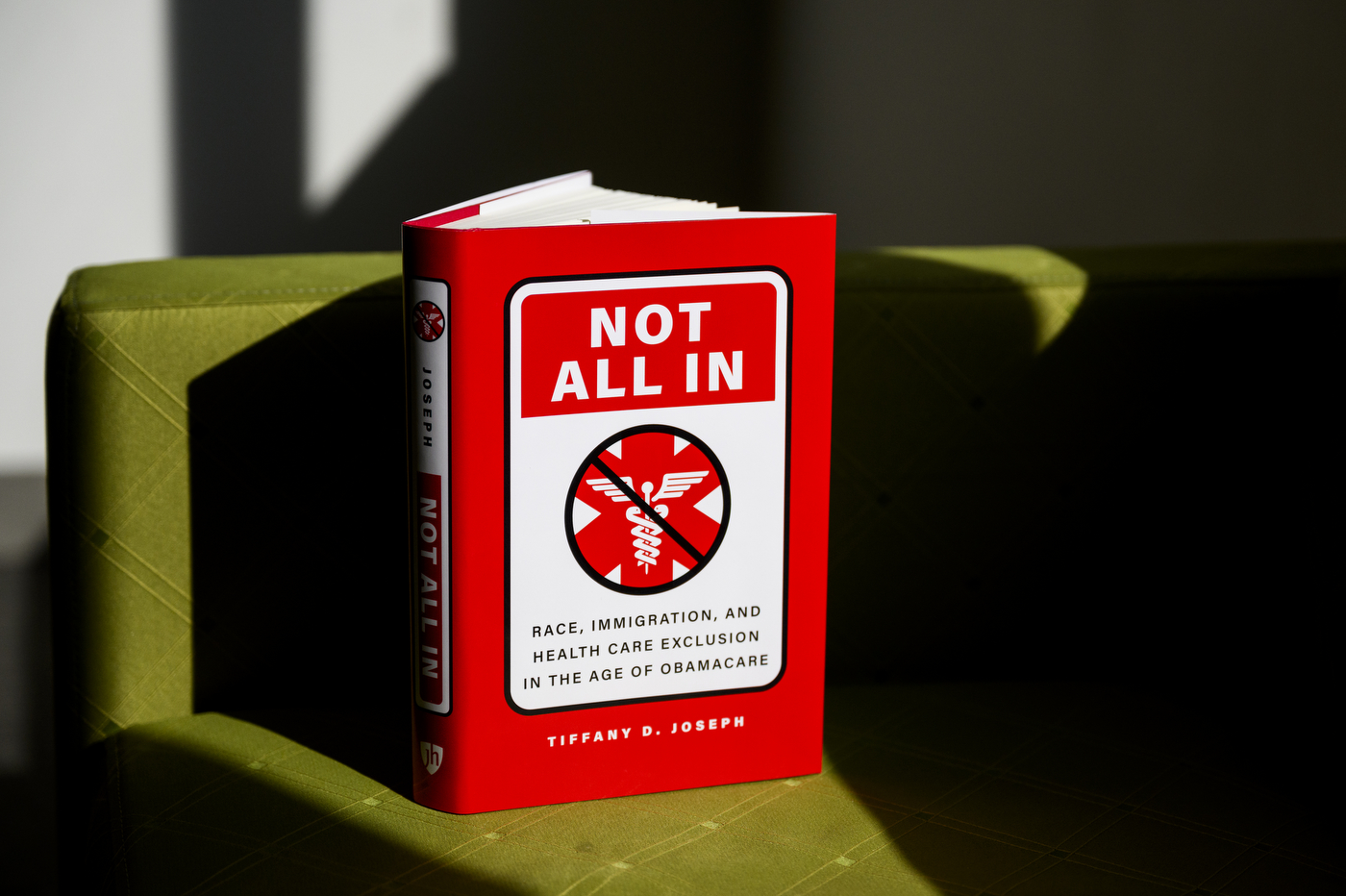
In a groundbreaking eight-year study, researcher Tiffany Joseph uncovered the complex barriers that race, ethnicity, and legal status create in accessing healthcare, revealing that having health insurance doesn't guarantee equal medical treatment.
Joseph's extensive research delves deep into the intricate challenges faced by marginalized communities, exposing how systemic inequalities can render health coverage ineffective for many individuals. Her work highlights the stark reality that insurance alone cannot overcome deeply rooted social and structural obstacles.
Through meticulous investigation, she demonstrated how factors like racial background, ethnic identity, and immigration status can significantly impact a person's ability to receive quality healthcare, even when they technically have medical coverage. These findings shed light on the invisible barriers that prevent many from obtaining the medical attention they need.
The study serves as a powerful reminder that healthcare access is about more than just having an insurance card—it's about navigating a complex system fraught with social, cultural, and institutional challenges that disproportionately affect vulnerable populations.
Joseph's research is a critical contribution to understanding healthcare disparities and provides valuable insights for policymakers, healthcare providers, and advocates working to create a more equitable medical landscape.
