Health Spotlight: Dallas County Shines as a Wellness Powerhouse in Iowa and Beyond
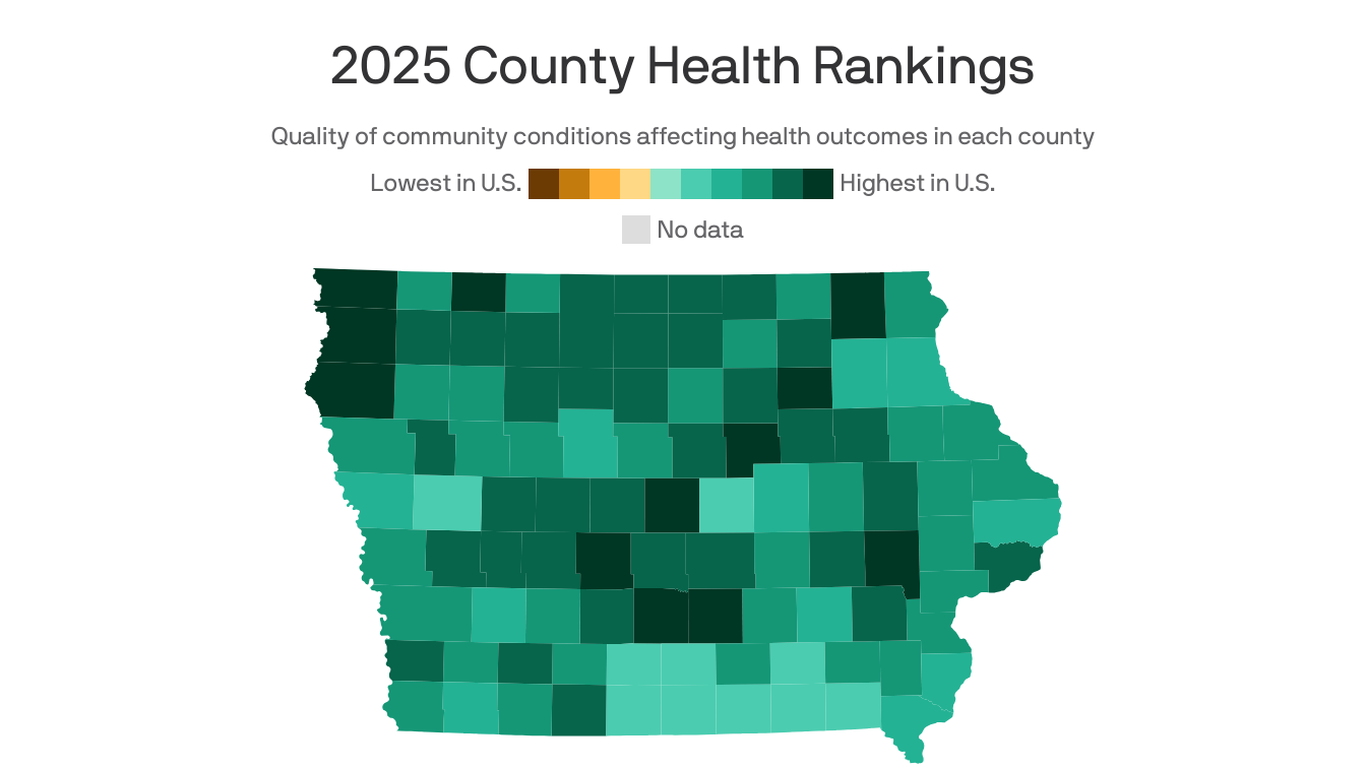
Dallas County Leads Health Rankings, Yet Disparities Persist for Rural and Minority Communities
While Dallas County shines at the top of regional health rankings, a closer examination reveals stark healthcare inequities that continue to challenge rural and nonwhite residents. The county's overall health metrics may look impressive on paper, but beneath the surface lies a complex landscape of unequal medical access and outcomes.
Recent comprehensive health studies highlight a troubling divide: despite the county's advanced medical infrastructure and resources, significant barriers remain for marginalized communities. Rural residents and people of color frequently encounter substantial obstacles in receiving timely, quality healthcare services.
Key challenges include limited healthcare facilities in remote areas, fewer preventive care options, higher rates of chronic disease, and systemic barriers that discourage medical engagement. These disparities are not just statistical abstractions but represent real-world struggles for thousands of residents seeking essential medical treatment.
Local health experts emphasize the urgent need for targeted interventions that address these systemic gaps. Proposed solutions range from mobile health clinics and community outreach programs to increased funding for underserved regions and culturally competent healthcare training.
As Dallas County continues to celebrate its overall health achievements, community leaders and healthcare professionals are increasingly focused on bridging these critical gaps, ensuring that quality healthcare becomes a reality for all residents, regardless of geographic or demographic background.
